- Home
- About Us
- Membership
- Advocacy
- Whitepapers & Reports
- Ohio Council PAC
- Find My Legislators
- Ohio Medicaid Matters
- The Ohio Association for the Treatment of Opioid Dependence
- Report: 2024 School-Based Summary
- Events
- News
- Resources
- My Profile
- Key Resources for Medicaid Billing
- Key Resources for Medicaid Next Generation Implementation
- Rules Governing OhioMHAS Certified Providers
- Job Bank
In December 2021, The Ohio Council of Behavioral Health & Family Services Providers published “Breaking Point: Ohio’s Behavioral Health Workforce Crisis,” an in-depth report on the employee recruitment and retention challenges faced by mental health and addiction services provider organizations. Based on original research and first distributed to the public in mid-February 2022, “Breaking Point” outlines how front-line clinical and medical staff are proving difficult to find, easy to lose, and costly to replace. As the report explains, the consequences could be grave for many Ohioans in need. Reporters and Media: Download the "Breaking Point" Press Release Click a header to jump to that section:
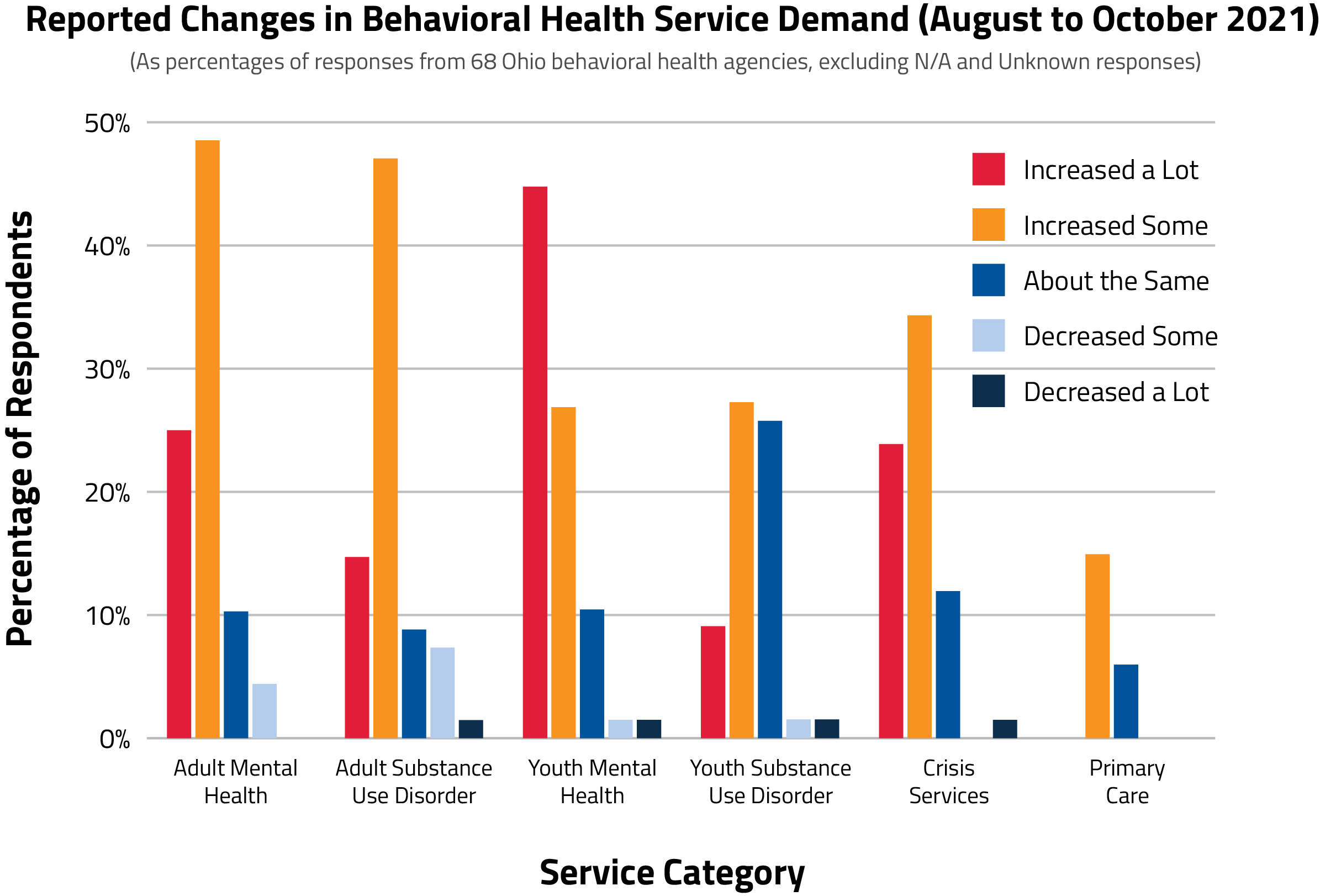
Questions about this report? Send an email to Training and Communications Director Erich Hiner at [email protected]. The Problem: Unprecedented Demand, Limited WorkforceDriven by stressors related to the COVID-19 pandemic and opioid overdose epidemic, demand for mental health and substance use disorder treatment is at an all-time high in Ohio. Data from the Ohio Department of Mental Health and Addiction Services show a 353% increase in demand for behavioral health treatment between 2013 and 2019. Demand rose sharply in 2020-21 and is anticipated to rise further by 2030. Of responding behavioral health care organizations to a survey conducted by The Ohio Council, more than 70% said demand for adult and youth mental health services increased from August to October 2021 (see below). More than 60% noted higher demand for adult addiction services, and more than 57% reported higher demand for crisis services.
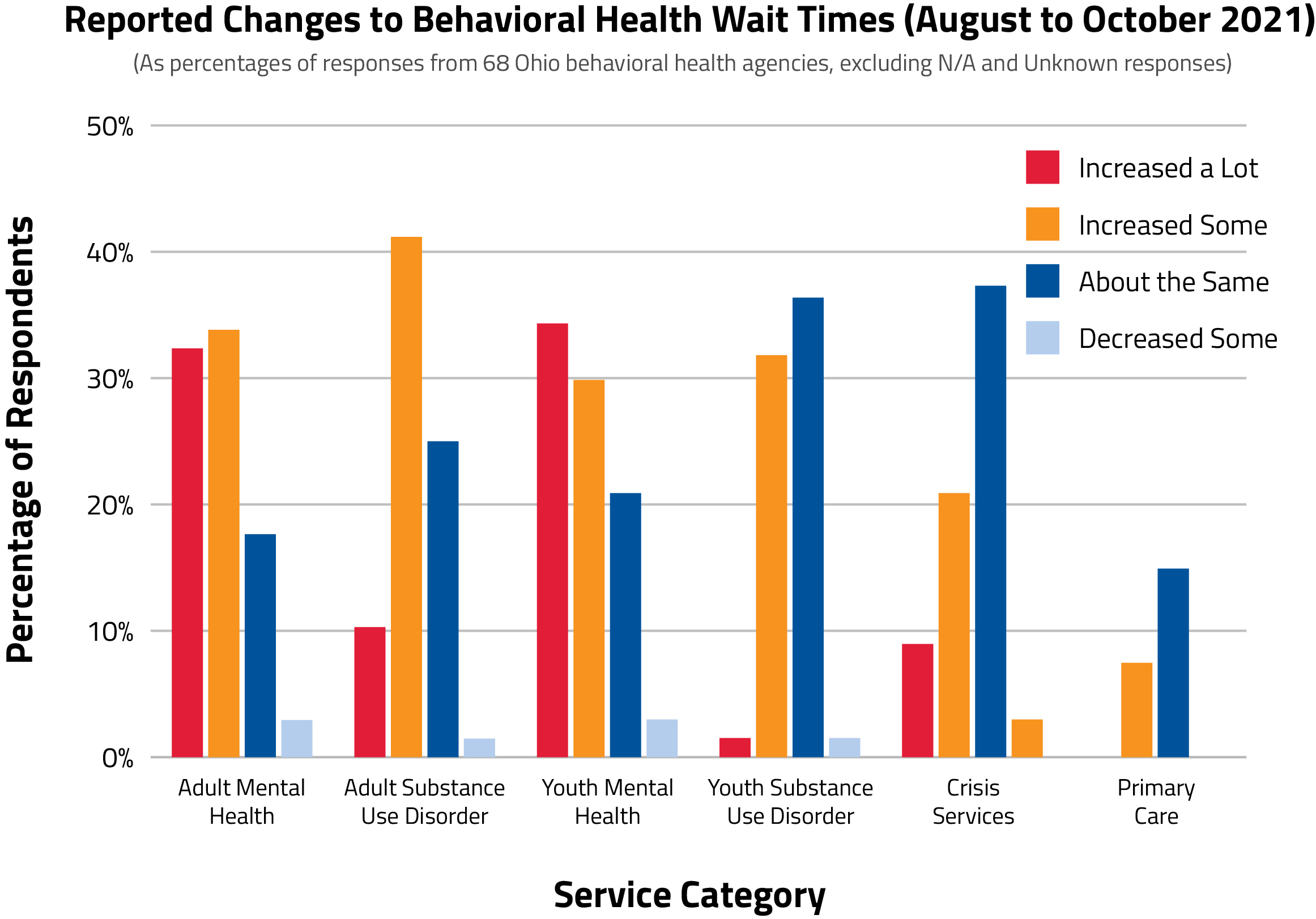
As demand rises, patients wait longer for critical services. More than 60% of survey respondents reported longer wait times for adult and youth mental health services from August to October 2021, and more than 50% reported longer waits for adult substance use disorder (SUD) treatment (see below).
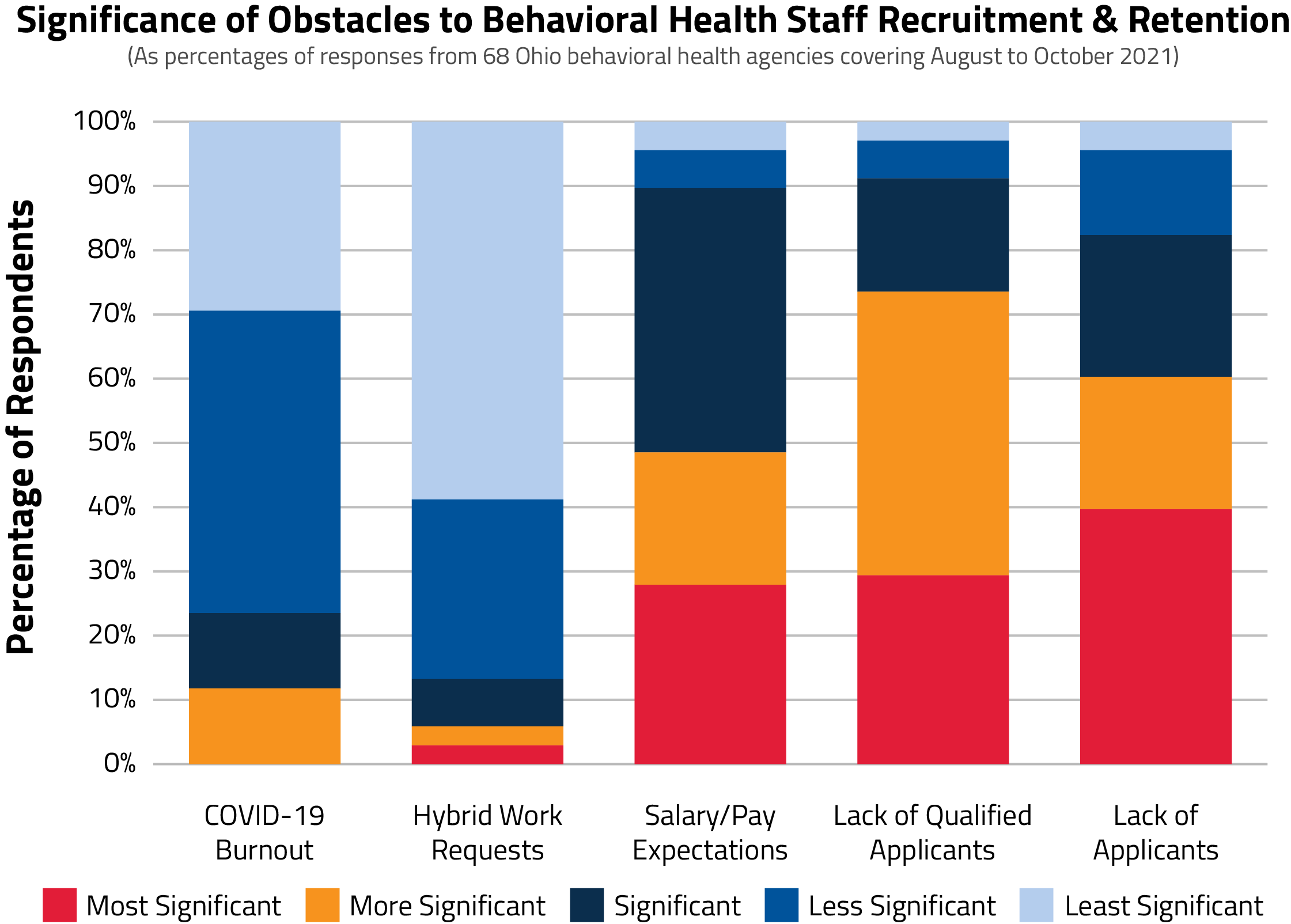
At the same time Ohioans’ need for treatment is rising, the behavioral health workforce is wearing thin. Ohio Council survey respondents report that front-line clinical and medical staff such as psychiatrists, therapists, and case managers are becoming harder to find in sufficient numbers to meet growing demand. When they can be found, front-line staff have become more likely to leave their jobs or to exit the field altogether. Once vacated, positions are staying open for longer, which widens the gap between treatment supply and demand. More than 98% of survey respondents said recruitment was very or somewhat difficult between August and October 2021. More than 88% reported difficulty keeping staff. Roughly 77% reported higher turnover with many positions open for two to six months, and more than 10% reported clinical/medical vacancies lasting for more than a year. More than 70% said a lack of qualified applicants is an obstacle to recruitment and retention, suggesting that credentialing requirements may be limiting the number of potential recruits.
Download the Full "Breaking Point" Report. The Causes: Attrition, Stress, Insurance Issues, and Credentialing Behavioral health workforce shortages have come about and worsened for several reasons. Natural attrition was an everyday reality in the field prior to the pandemic. Behavioral health care is often stressful with long, irregular hours and on-call requirements. In addition, community-based practice often requires practitioners to navigate emotionally taxing and high-risk situations. 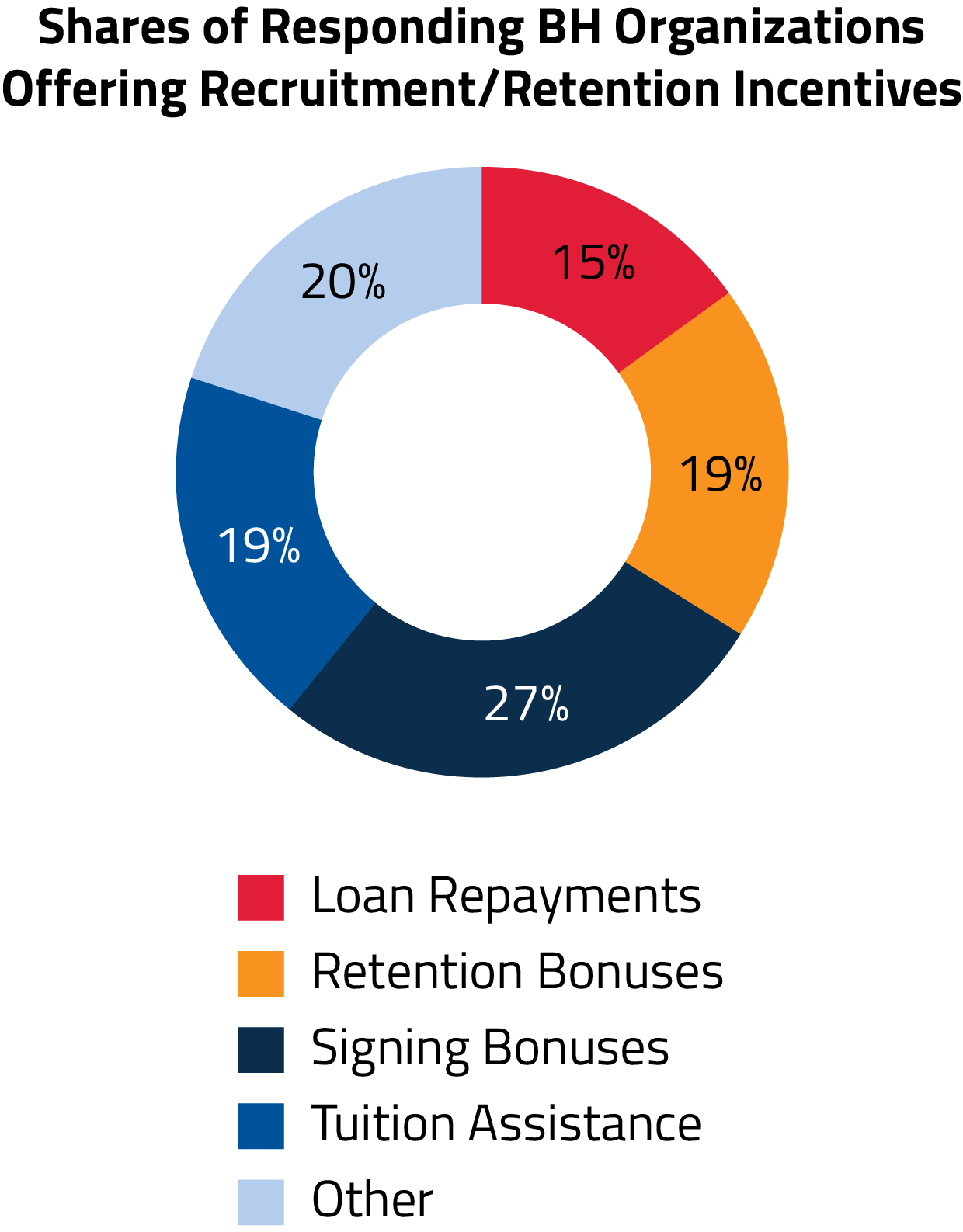
Pandemic stress has worsened these factors in recent years. As practitioners face longer hours and tough questions at home related to COVID-19, existing attrition issues have worsened. This has also been exacerbated by a lack of professional value. Many report feeling unrecognized as the critical health care workers they are. This feeds job stress, limits the workforce, and lengthens wait times for patients as a result. Turnover is also due in part to an uncompetitive pricing market resulting from insufficient insurance coverage and reimbursement. While many private insurance companies cover behavioral health, many do not cover a full range of services for acute and chronic care or do not recognize all available licensed professionals. If an insurer does cover these essential services, it is likely at an inadequate rate. Ohio Medicaid, meanwhile, is limited to reimbursing for services at a rate that often falls below the actual cost of care. The gaps left by inadequate private-sector payments and coverage of services and providers have contributed to wage stagnation. These trends are colliding at a time when many large, private employers are rolling out significant incentives to attract new workers. Most companies are not limited by the same reimbursement issues as behavioral health providers, which means providers often cannot adequately compete for workers despite creative retention efforts (see chart). Lastly, recruits are being kept out of the system by excessive professional licensing and education requirements. State rules often require a person to have a master’s degree to hold behavioral health licensure, and earning potential is limited in the field below that level of education. As a result, the industry lacks a clear career ladder. More numerous and less costly points of entry and career growth paths are necessary to increase the workforce and meet demand. Download the Full "Breaking Point" Report. The Solutions: Relief, Parity, Simplicity, and Administrative ReformAs more Ohioans require and seek behavioral health care, the workforce must be available to handle the rising demand and provide services to those in need. If the crisis remains unaddressed, Ohioans who need mental health and addiction services may go without them and, in some instances, need to escalate to crisis services to access care. The Ohio Council recommends the following to address the workforce shortage: Short-Term: Targeted Relief & Infrastructure Development
Short-Term: Enforce Existing Parity Requirements
Short-Term: Remove Administrative Barriers
Mid-Term: Develop New Reimbursement & Licensure Models
Long-Term: Strengthen the Workforce Pipeline
Download the Full "Breaking Point" Report. Conclusion and Acknowledgments The community behavioral health workforce is at its breaking point. The behavioral health workforce crisis was a growing cause for concern prior to 2020 and has only worsened since the pandemic began two years ago. The demand for employees across the economy has led to increased starting wages and improved benefit packages that are nearly impossible for non-profit organizations to compete with due to perceived lack of value of the work, challenging and unpredictable work settings and schedules, and insurance reimbursements that are static and do not keep pace with inflation or the cost of doing business. In addition, administratively burdensome regulations and licensure make it difficult for behavioral health care providers to recruit and sustain an adequate workforce. As the demand for behavioral health services continues to increase, so does the need to recruit and retain qualified staff. The current shortage of skilled and highly trained workers requires immediate planning and action to ensure that Ohio can meet current demand, adapt to consistently growing behavioral health needs, sustain access to a full continuum of care, and provide quality services across the state. We must act now to build career pathways and a workforce pipeline that brings young and aspiring talent into these professions. The Ohio Council of Behavioral Health & Family Services Providers would like to thank our member organizations that responded to our 2021 workforce survey. This report was made possible by the time and care taken by agency staff in providing reliable, recent employment data. We would also like to thank Ohio Governor Mike DeWine, RecoveryOhio, the Ohio Departments of Medicaid and Mental Health & Addiction Services, and other executive agencies for their ongoing efforts to improve access to mental health and substance use disorder treatment throughout the state. Download the Full "Breaking Point" Report. Questions about this report? Send an email to Training and Communications Director Erich Hiner at [email protected]. The Workforce Crisis and "Breaking Point" in the News
|