- Home
- About Us
- Membership
- Advocacy
- Whitepapers & Reports
- Ohio Council PAC
- Find My Legislators
- Ohio Medicaid Matters
- The Ohio Association for the Treatment of Opioid Dependence
- Report: 2024 School-Based Summary
- Events
- News
- Resources
- My Profile
- Key Resources for Medicaid Billing
- Key Resources for Medicaid Next Generation Implementation
- Rules Governing OhioMHAS Certified Providers
- Job Bank
| OhioRISE Provider Manual Now Available |
|
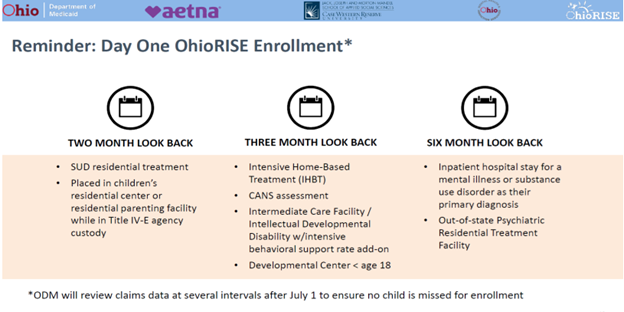
ODM released the OhioRISE Provider Enrollment and Billing Guidance (AKA OhioRISE Provider Manual) in late May with an effective date of July 1. ODM shared the following statement in their announcement of the release, “The OhioRISE program covers a range of behavioral health (BH) services for youth that are comprised of existing, enhanced, and new behavioral health and care coordination services. This guide is intended to share policies related to billing for the new and enhanced OhioRISE services. Existing behavioral health services will be covered in accordance with the OhioRISE Mixed Services Protocol and will be billed consistent with the billing policies outlined in the appropriate provider type billing guidelines.” The OhioRISE Provider Enrollment and Billing Guidance document offers a summary of operational information to support providers with implementation. It covers practitioner enrollment, prior authorization and approval, CANS, and the new services. The manual offers additional details on claims structure, including the expectations to use the full complement of practitioner modifiers. To clarify, youth enrolled in OhioRISE will have all behavioral health services covered and reimbursed by Aetna OhioRISE. The youth’s physical healthcare services will remain covered by the traditional Medicaid managed care plan. OhioRISE includes both a “day one” enrollment based on the youth’s previous utilization of inpatient psychiatric services, PRTF, IHBT, ICF/DD with BH add-on payment, developmental center placement <age 18, SUD residential, and placement in a children’s residential center or parenting facility while in Title IV-E agency custody. (See slide below). Initially, ODM estimates around 5,300 youth will be enrolled in OhioRISE on day one. On-going, enrollment into OhioRISE will be mandatory for youth that meet the OhioRISE eligibility based on the CANS or for those entering an inpatient level of care for a behavioral health condition or PRTF. Enrollment will occur on the date the youth’s CANS score is entered into the CANS IT database or admission to an inpatient unit or PRTF and can occur at any time during the month. Youth who do not meet the OhioRISE eligibility will continue to have their behavioral health services covered by their Medicaid MCO.
|